Abstract
Introduction: Response to chemotherapy treatment both by cytology and by more sensitive techniques such as cytometry is one of the most influential parameters in the survival of patients with Acute Myeloid Leukaemia (AML). Patients with detectable minimal residual disease (MRD) or those with active disease (AD) after induction or prior to allogeneic transplantation (HCST) represent a high-risk group.
Objectives: to analyse the impact of disease burden before HSCT in terms of Overall Survival (OS) and Event Free Survival (EFS) in a group of patients who received HSCT in a single institution. We also analysed the influence of disease burden at the end of induction (considering best response after 1 or 2 cycles) and its impact on those patients in Cytological Remission (CR) with MRD <0.1% prior to transplantation.
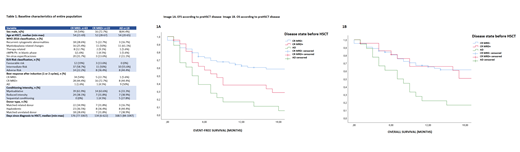
Methods: We analysed 103 patients who received HSCT in one centre between 2008 and 2020 in whom we knew disease status after induction and before HSCT. We divided the cohort into three groups according to preHSCT disease: Group 1) Patients in CR with MRD <0.1% by cytometry, Group 2) CR with MRD ≥0.1% and Group 3) patients with AD (≥5% blasts by cytology). We analysed post-transplant EFS and OS using the Kaplan Meier method and the Cumulative Incidence of Relapse (CIR) using Gray's test.
Results: The baseline characteristics of the population are reflected in table 1. Median follow-up was 13 months (0-140). One-year EFS (1y-EFS) was 49%. One-year OS (1y-OS) was 57.5%, with a 1y-IAR of 27%. We first analysed the impact on post-transplant survival according to the different groups. Group 1 had significantly better EFS than Group 2 (p=0.04) and Group 3 (p<0.001) (Figure 1A). Regarding OS there was no difference between Group 1 and Group 2 (p=0.2) although it was significantly better than Group 3 (p<0.001) (Image 1B). IAR-1 was 14% vs 48% vs 50% (p<0.001) respectively. We subsequently analysed the impact on post-transplant survival according to the response to induction. Post-transplant EFS and OS were better in those in CR MRD- after induction compared to patients in CR with MRD+ (p=0.05 and p=0.002) as well as in patients with AD at the end of induction (p=0.002 and p=0.008). We stratified Group 1 according to the best response to induction (MRD- or MRD+/EA) and we performed an analysis according to the following groups: A) Patients with MRD- after induction and also before HSCT, B) Patients with MRD+/EA after induction achieving MRD- before HSCT. Comparing both groups there were no differences in either EFS (1y-EFS Group A 69% vs Group B 54%, p=0.5) or OS ( Group A 69% vs Group B 61%, p=0.8).
Conclusions: Patients with pre-transplant AD or MRD+ are a high-risk group due to a high incidence of post-HSCT relapse. Although patients with AD or CR with MRD+ after induction have a worse prognosis, those who achieve MRD- before HSCT have a similar survival to the MRD- group from the start of chemotherapy.
Garcia-Gutiérrez: Pfizer: Research Funding; Bristol-Myers Squibb: Consultancy; Incyte: Consultancy; Novartis: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal